According to the Centers for Disease Control and Prevention (CDC), more than 25,000 infants die each year in the United States. Infant mortality is defined as the death of an infant before one year of age. Infant mortality rates refer to the number of infant deaths for every 1,000 live births. The infant mortality rate in the U.S. is six deaths per 1,000 live births and is worse than that of many other industrialized countries (CDC, 2013).
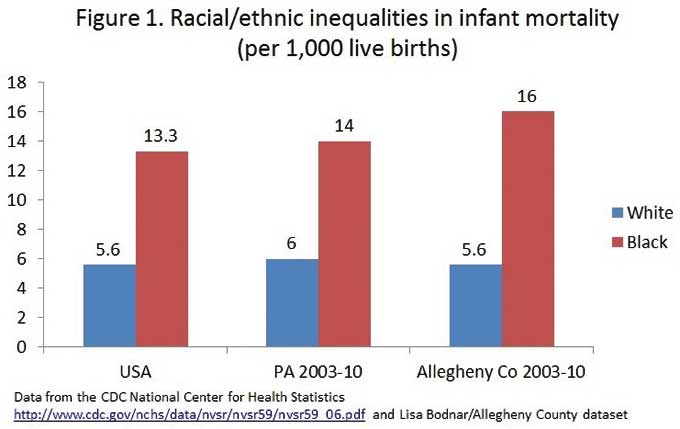
Infant mortality rates vary by the race of the mother. Sadly, the racial disparities seen in infant mortality rates between African Americans and Whites in Allegheny County are striking (Figure 1). In Allegheny County in 2009, there were 16 deaths per 1,000 live births among African Americans, while the rate among whites was 5.6 deaths per 1,000 births. The Allegheny County numbers for African Americans are considerably higher than both the state (14.4 deaths per 1,000 births) and national rates (11.6 deaths per 1,000 births). Disparities are also seen between African Americans and Whites on low birth weight (infants born weighing less than 5.5 pounds) and preterm birth (birth before 37 weeks of pregnancy). These are two of the major predictors of infant mortality.
The racial disparities in infant mortality rates are puzzling. It’s not clear what factors contribute to the differences. For example, take the complex problem of preterm birth. Differences in maternal characteristics, such as socioeconomic status, prenatal care, infection and nutrition, are known to contribute to disparities in preterm birth. But, in the U.S., African American women with advanced schooling are more likely to have an infant die in the first year than are White women who did not finish high school. The reasons for this disparity are not clear. Could other factors (like neighborhood environment) be contributing to the differences? Research is now focusing on the role of stress as one key contributing factor.
The Community Child Health Network (CCHN) is a large, federally funded research project currently underway to help understand how communities and families create a context that influences pregnancy and infant and child health. The goals of this research include looking at how community, family and individual stressors can influence and affect pregnancy health. Researchers are also studying whether these factors might result in health disparities in pregnancy outcomes and infant mortality. Although the CCHN study does not include Pittsburgh, the results from this research will provide valuable insights into ways to reduce infant mortality rates and to effectively address racial disparities in pregnancy outcomes. More information about the CCHN project can be found at https://www.communitychildhealthnetwork.com/index.html.
Researchers are now interested in interventions are being planned that adopt a holistic (consideration of the complete person, physically and psychologically) approach and focus on health across the entire lifespan, not just when a woman is pregnant. Reducing disparities in infant mortality and improving birth outcomes will require an increase in efforts to better understand the reality of African American women’s lives, both during pregnancy and overall.