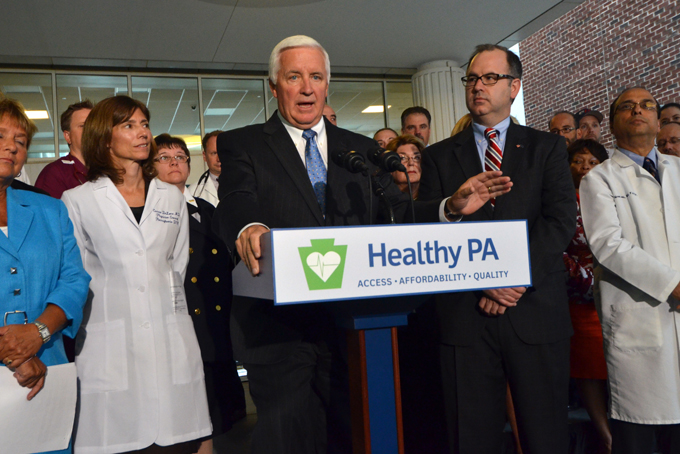
Gov. Tom Corbett announces that he will seek federal Medicaid expansion money to extend health insurance to an estimated 520,000 working-age adults, although he also outlined a list of conditions under which he would accept the money, Monday, Sept. 16, 2013 in Harrisburg, Pa. Corbett made the announcement in a news conference at Harrisburg Hospital, flanked by aides, supporters and personnel from the hospital and PinnacleHealth. (AP Photo/Marc Levy)
Though congress has exempted itself, the judiciary branch and executive branches of the federal government, and the president have unilaterally postponed its mandate for businesses to provide employee coverage for one year, beginning Oct. 1, the Affordable Care Act requires that all individuals purchase health insurance.
In Pennsylvania, residents will be able to buy insurance through federal healthcare exchanges. These were expected to be up and running already, but as of last week, the U.S. Department of Health and Human Services had only made insurance carrier filings (identifying what companies you may purchase from) in 13 states and the District of Columbia. Pennsylvania is not among them.
Kathleen Sebelius, HHS secretary, has said she will release the data for the remaining participating states Sept. 19.
Broadly speaking, uninsured residents with incomes above the poverty line ($23,500—$94,000 for a family of four) will qualify for a subsidy to purchase either Bronze, Silver, or Gold plans, each with different levels of coverage, deductibles and co-payments.
Using a calculator developed by the Kaiser Foundation, online at https://kff.org /interactive/subsidy-calculator/, individuals can determine their subsidy level.
In general, a household with two non-smoking adults (say, age 30 and 28) and two minor children, an income of $25,000 (106 percent of the poverty level) and no employer provided coverage would be eligible for a $10, 039 subsidy, which covers 95 percent of the $10,539 unsubsidized Silver-Level insurance plan, and would only pay $500 in annual premiums. Deductibles and co-payments will vary from plan to plan but, under the above scenario, out-of-pocket expenses, other than the premium, would be capped at $4,500.
However, in Pennsylvania, children are covered by CHIP, so the above formulation would yield a $6,206 subsidy on a premium of $6,706—again a $500 difference. Smoking, though, would raise the unsubsidized premium to $10,059, for an annual cost of $3,853.
In states that agreed to expand Medicaid, the hypothetical family above—or any household with income up to 138 percent of the poverty level—would be covered under Medicaid, and would see lower premiums, deductibles and co-payments.
The most recent U.S. Census data indicates the poverty rate for Allegheny County at 12.4 percent. For Pittsburgh, the poverty rate is 22 percent. And according to a recent Pittsburgh United report, that rate is 31 percent for working-age African-Americans.
Pennsylvania Gov. Tom Corbett, one of several who sued over the legality of the ACA, initially said the state would not expand Medicaid even though the federal government pledged to cover 100 percent of the increased cost through 2016 and 90 percent thereafter.
He reversed himself Sept 16, sort of. Corbett said the state would expand coverage “if and only if” the federal government approves a plan to reform the current Medicaid system.
Corbett’s proposal is to purchase a “premium assistance model” that would provide subsidies to 520,000 low-income individuals so they can buy coverage from the new exchanges. Even if the plan is approved, state officials have no idea when it could be in place.
Without Medicaid expansion, the state would likely see a raft of hospital closings next year when the federal government eliminates its “disproportional share” payments meant to compensate for treating uninsured patients. The federal Medicaid expansion funds would cover most of those patients.
However, it remains to be seen how much coverage ACA consumers will have. The Los Angeles Times reported Sept. 14 that the insurers in its exchanges are limiting the number of hospitals and doctors available to ACA patients from one-third to one-half as many as those available to employer-provided plans to hold down costs.
In West Virginia, rather than spurring competition to hold down prices, the ACA has inadvertently spawned a monopoly, as Highmark Blue Cross Blue Shield will be the only provider offering coverage through its exchanges.
Additionally, though the ACA coverage goes into effect Jan. 1, the open enrollment period runs through March. Those who do not enroll will face penalties levied by the IRS. The agency finalized the regulations last month. Though there are exceptions, the fine (for each uninsured individual) is either: $95 in 2014; $325 in 2015; $695 in 2016, or 1 percent of taxable household income, rising to 2 percent in 2015 and to 2.5 percent thereafter.
(Send comments to cmorrow@newpittsburghcourier.com.)
Your comments are welcome.
Follow @NewPghCourier on Twitter https://twitter.com/NewPghCourier
Like us at https://www.facebook.com/pages/New-Pittsburgh-Courier/143866755628836?ref=hl
Download our mobile app at https://www.appshopper.com/news/new-pittsburgh-courier