According to the U.S. Department of Health and Human Services, rates of sexually transmitted infections (STIs) reached an all-time high in 2018 among both females and males and all racial and ethnic groups (data about people who are nonbinary were not available). With the release of the first-ever STI National Strategic Plan in late 2020, the United States began a path toward preventing the spread of STIs and effectively treating them.
STIs are a significant public health concern. Left untreated, STIs can spread to greater numbers of people and can lead to pelvic inflammatory disease, infertility, poor birth outcomes and an increased risk of getting HIV and certain cancers. People with STIs can experience stigma and discrimination, which can diminish their quality of life.
The number of diagnosed STIs has been rapidly rising in recent years. The Centers for Disease Control and Prevention (CDC) reports that the number of combined cases of gonorrhea, syphilis and chlamydia was more than 2.4 million in 2018 and that half of these STIs are among youths. Adolescents and young adults, men who have sex with men and pregnant women are disproportionately affected by STIs. Black, American Indian/Alaska Native and Hispanic/Latinx communities also carry a greater burden of STIs.

ASHLEY HILL, DRPH, MPH
Ashley Hill, DrPH, MPH, assistant professor of epidemiology at the University of Pittsburgh’s Graduate School of Public Health, studies the determinants of STIs in people ages 15-24 and how to best support this population.
“I focus on this population because they carry a significant burden of STIs in the United States and also in Allegheny County,” says Dr. Hill. “Nationally and locally, that age group composes about 50% of all STIs each year. All STIs are preventable and most are treatable and can be caught early.”
Dr. Hill has examined the causes of young people’s greater risk for STIs and found that there are different factors that influence their sexual and reproductive health and their ability to make safe decisions and adopt healthy practices. Some of those factors include the inability to access health care or insurance, condoms or confidential screening for STIs. Structural racism in past and current health care settings and its effects on health care use and access are also factors. Unequal power dynamics or intimate partner violence can take away people’s autonomy when making decisions about their bodies, sexual health or reproductive choices. Also, in the United States as a whole, Dr. Hill points out that some people experience shame and have difficulty discussing healthy sexuality and relationships, which can lead to young people having fewer opportunities to make informed decisions.
“We need to push information more with young people,” says Dr. Hill. “We need to use information that is correct, culturally appropriate and that makes sense for the age group. We also need to introduce topics like healthy sexuality and relationships at an earlier age in the greater context of overall health and well-being.”
A vital part of providing more information to young people about STIs, sexual health and reproduction is asking them how they would like to be supported.
“We need to move toward integrating young people’s wants, needs and desires into the programs we’re pushing for,” she says. “We want to know what works for them, what their concerns are, what adults in their lives can do to support them and how to help them be heard. We want to help provide actionable change that improves their lives.”
Currently, Dr. Hill and colleagues are also looking at the effects of sexual violence on STIs through research on Black women’s experiences of sexual misconduct at the University of Pittsburgh. They’re seeking to understand barriers to reporting such incidences and how Pitt can best support people who have had these experiences. The study—Black Women in Academia (BWA): Supporting Healing and Empowering—has implications for STIs because, if someone has experienced sexual misconduct or violence, that person could be at risk for an STI.
Though more research is necessary, Dr. Hill says that STI spread has continued through the COVID-19 pandemic. Because many people were not able to keep regular wellness appointments and have fallen away from getting routine exams, the concern is that there are even more undiagnosed and untreated STIs. During the pandemic, most young people have been out of school for months and lost various touchpoints, whether those are school or other social support services. Dr. Hill says health care providers’ offices have instituted COVID-19 prevention practices, and she encourages people to keep health and wellness appointments.
Dr. Hill says that a broader goal is to put in place mechanisms to support reproductive-age people to have healthy relationships and to engage in sex in a way that makes sense for them but also is not contributing to infection, disease or adverse effects on well-being overall.
The Allegheny County Health Department provides confidential screening services and treatment for STIs at its clinic. For more information, please visit https://www.alleghenycounty.us/Health-Department/Health-Services/STD-and-HIV-AIDS-Program/index.aspx.
For more information about the BWA study, email bwa@pitt.edu.
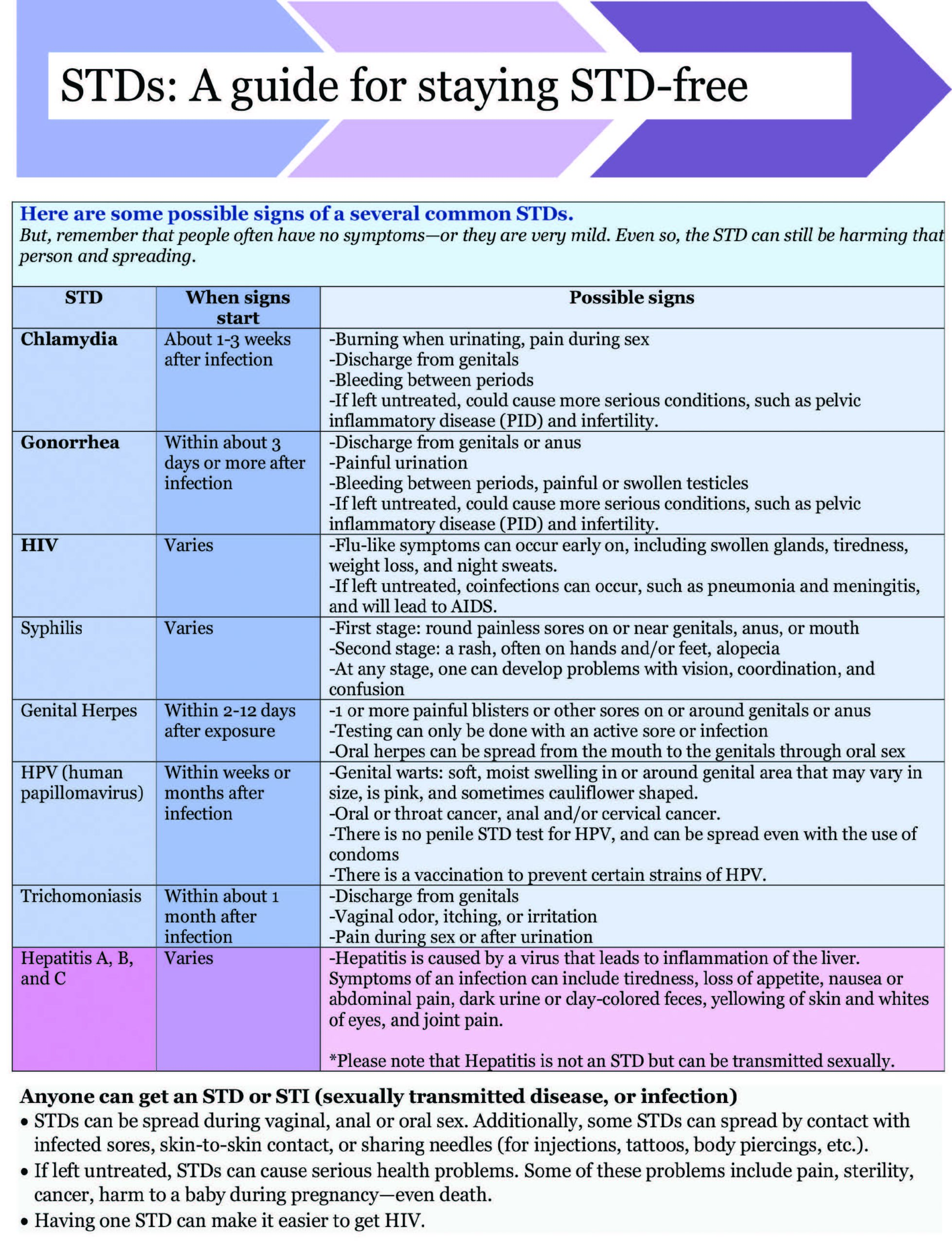
Chart courtesy of Allegheny County Health Department’s Public Health clinic.
