In the U.S., about 1 in 5 children and adolescents have obesity, according to the CDC. Having obesity means a child’s weight is a lot higher than what’s typical for their height, age, and sex. Healthcare providers use a body mass index (BMI) chart to determine who has obesity.
Like other health conditions caused by social inequities, obesity affects some groups more than others. It’s highest in Hispanic and Black children and lowest in White and Asian children.
Children who have obesity are more likely to develop health conditions like type 2 diabetes, high blood pressure, high cholesterol, liver and gallbladder diseases, and joint, breathing, and digestive problems.
A child’s mental health can also be affected. Children who have obesity often face bullying, discrimination, and stigma about their weight.
All these physical and mental health conditions can begin in childhood and continue throughout adulthood. That’s why it’s important to offer healthcare support to children and their families early.
MARY ELLEN VAJRAVELU
University of Pittsburgh’s Dr. Mary Ellen Vajravelu, Assistant Professor of Pediatrics and Epidemiology, studies and treats childhood obesity, especially as it impacts diabetes. She’s found that a good approach to treating the condition — one that works over time — includes family support, healthcare education and tools, and listening skills.
“The goal is for healthcare providers and family members to make the focus on the child’s health and health behaviors — not just weight,” she says. “Making healthy, sustainable lifestyle changes works best when the child and family embrace a health plan as a team.”
In helping the family create a plan, healthcare providers should look first at the child’s physical activity, nutrition, mental health, and family history. “It’s about lifestyle,” says Dr. Vajravelu. “You want to help the child build a tool kit they can carry with them for lifelong health.”
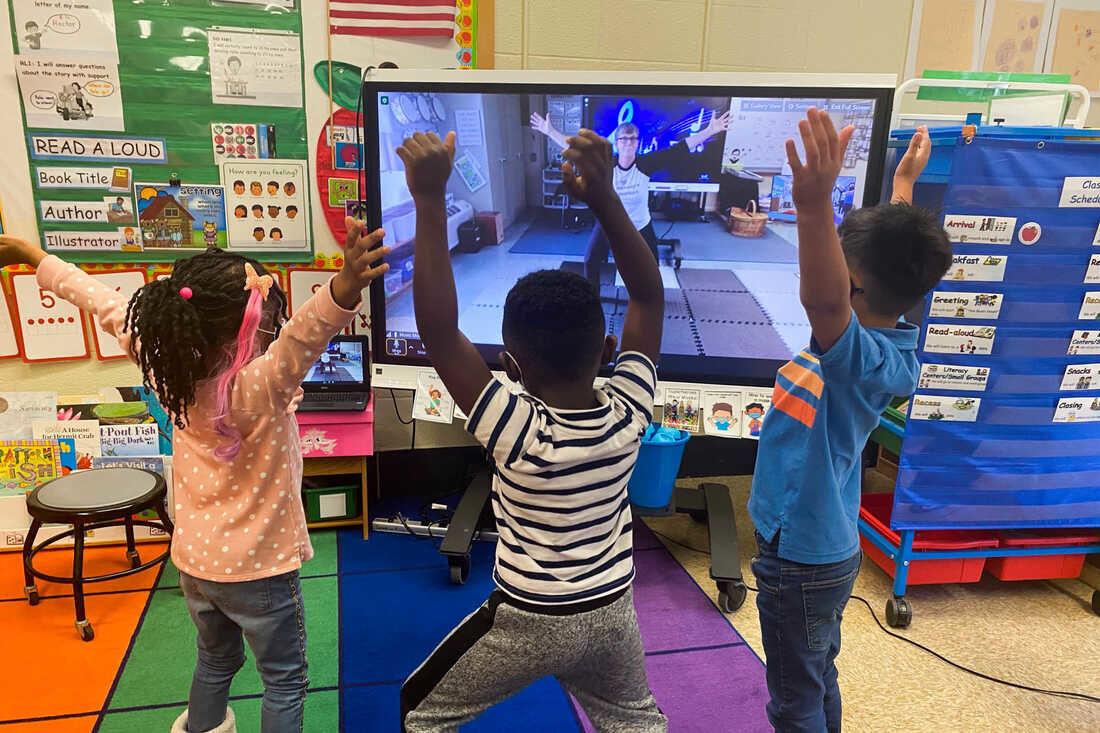
In addition to healthy lifestyle changes, the tool kit could include medicine to treat diabetes, high blood pressure, or high cholesterol. It might consider family mental health counseling for depression, anxiety, or an eating disorder. It could suggest social media apps for 10 minutes of daily exercise, like TikTok dances, jumping jacks, or a brisk walk with a family member or friend. It might add a referral to a local food bank or vouchers for a community garden or farmer’s market for fresh fruits and vegetables.
One low-tech tool for good health is for everyone in the family to pay attention to food labels, especially added sugar. “Learning how much sugar is too much is eye-opening for a lot of people,” says Dr. Vajravelu. “Just cutting out sugar-loaded drinks like pop can have an immediate and positive impact on health.”
Portions, too, are a good starting point for better health, especially cultural comfort foods. “Completely giving up foods you love, especially foods you eat during holidays and family gatherings, isn’t going to work over time,” notes Dr. Vajravelu. “Instead, we encourage our patients and families to think about comfort food in terms of smaller portions less often, but just as joyful.”
A new tool that’s receiving a lot of media attention is GLP-1 medications, such as Ozempic and Wegovy. Weekly shots of these medications regulate blood sugar, slow digestion, and reduce people’s appetites. Common side effects include gastrointestinal issues like nausea, diarrhea, and vomiting.
GLP-1s are approved for managing type 2 diabetes and for helping people with obesity, including children and adolescents. Currently, Pennsylvania Medicaid insurance plans cover GLP-1s for children, though it is possible that may change with budget cuts. For other types of insurance that offer coverage, out-of-pocket prices vary but can be hundreds to over a thousand dollars per month.
In her practice, Dr. Vajravelu educates patients and their families about GLP-1s, noting that many families bring it up themselves. “A family member may have had their own successful GLP-1 weight loss and they’re curious about it for their child,” she explains. “We discuss what we know from a research standpoint about short-term side effects, including stomach upset and possible gallbladder pancreas issues.”
Long-term side effects are still unknown. “They haven’t been studied yet for children,” says Dr. Vajravelu. “We also don’t know an easy way for people to go off GLP-1s without gaining back most of weight they lost.”
She continues, “There are other appetite suppression drugs that have been studied over a longer period and with different side effects. GLP-1s are just the latest. Like the others, they’re not safe to start without also making healthy lifestyle changes together.”
Currently, Dr. Vajravelu is studying how adolescents with obesity who’ve been prescribed GLP-1s feel about the new drug. “Despite some of the side effects, the word we keep hearing is ‘hope,’” she says. “These adolescents feel hopeful about building a healthier future for themselves. As a doctor, researcher, and someone who cares deeply about equitable public health, that’s a good feeling.”